Molluscum contagiosum (MC) is a self-limited infectious dermatosis.
It is caused by molluscum contagiosum virus (MCV) which is a double-strand DNA virus which belongs to the Poxviridae family. MCV has 4 different genotypes: MCV 1, MCV 2, MCV 3, and MCV 4. MCV 1 is the most common genotype (75–96%), followed by MCV 2, while MCV 3 and 4 are extremely infrequent.
MCV infects the epidermis and replicates in the cytoplasm of cells with a variable incubation period between two and six weeks.
Molluscum contagiosum is transmitted mainly by direct contact with infected skin, which can be sexual, non-sexual, or autoinoculation. Additionally, it can be transmitted by contaminated fomites like bath sponges or towels.
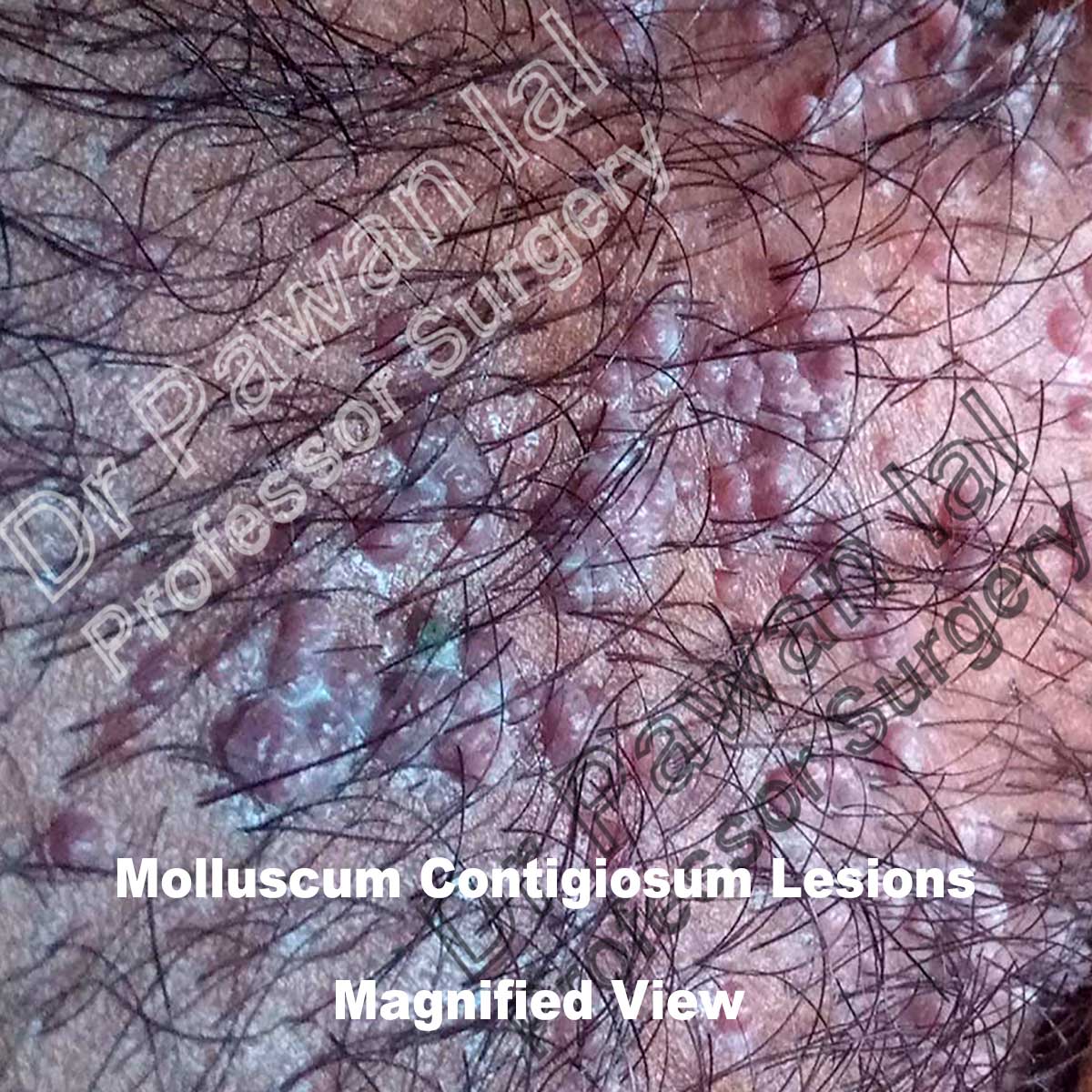
Clinically, MC presents as firm rounded papules, pink or skin-colored, with a shiny and umbilicated surface. Patients infected with MCV present firm rounded papules from 2 to 5 mm, pink or skin-colored, with a shiny and umbilicated surface. The lesions may be single, multiple or clustered, and occasionally they may have an erythematous halo or be pediculated. Pruritus may be present.
In adults, lesions are most frequently located in the lower abdomen, thighs, genitals, and perianal area, most of the cases transmitted by sexual contact.
The duration of the lesions is variable, but in most cases, they are self-limiting in a period of 6 to 9 months; however, some cases may persist for more than 3 or 4 years. It has described a phenomenon called “beginning of the end” (BOTE) sign which refers to clinical erythema and swelling of an MC skin lesion when the regression phase begins. This phenomenon is likely due to
an immune response towards the Molluscum Contigiosum virus infection.
The diagnosis of MC is clinically based on the distinguishing characteristics of the lesions. A useful clinical tool in the diagnosis of MC is dermoscopy, which enables us to observe structures not seen by the naked eye with a 10X magnification. MC display characteristic findings under the dermatoscope: a central pore or umbilication, polylobular white-to-yellow amorphous structures, and peripheral crown vessels.
If the diagnostic doubt persists, confocal microscopy or skin biopsy could be performed. The histopathological study is indicated when the diagnosis is not clear. The characteristic findings correspond to large intracytoplasmic eosinophil inclusion bodies known as Henderson-Petterson bodies.

Molluscum Contigiosum lesions in pubic region in male

Typical umblicated lesions of Molluscum Contigiosum
The differential diagnoses include mainly inflammatory, infectious, and neoplastic etiologies. In immunosuppressed patients, the main differential diagnosis includes histoplasmosis and cryptococcosis which can be seen as umbilicated papules
Infections
Verruca vulgaris
Chickenpox
Folliculitis
Condyloma acuminatum
Tumors
Syringomas
Steatocystoma multiplex
Basal cell carcinoma
Miscellaneous
Acne vulgaris
Milia
Treatment of Molluscum Contigiosum
Although resolution is ultimately spontaneous, scarring may occur, particularly if the lesions are secondarily infected. Thus there may be justification for active intervention in the hope of speeding resolution and hence limiting scarring, transmission, and the period of social exclusion.
Early treatment of infection may limit the spread of lesions by autoinoculation. Early active treatment could thus reduce the duration of infection and the degree of individual scarring and further transmission.
There are several treatment modalities which include mechanical, chemical, immunomodulatory, and antivirals.
It should be advised not to scratch or rub the lesions; besides, patients should not share towels, tub, or bath utensils.
Mechanical methods
Physical expression by squeezing:
physical expression by squeezing
Cryotherapy - is an effective treatment. It can be applied with a cotton-tipped swab or by portable sprayers, 1 or 2 cycles of
10 to 20 seconds are typically used. The disadvantages of cryotherapy are the possibility of blistering, scarring, and post-inflammatory hypo or hyperpigmentation.
Curettage - is also an effective method and involves the physical removal of skin lesions. It can be done with a curette, punch
biopsy, needle or with an ear speculum. To reduce pain, topical application anaesthesia is used. Curettage can cause pain, bleeding, and scarring. After curettage, topical povidone iodine is applied. This is an antiseptic useful in the treatment of Molluscum Contagiosum.
Chemical Methods
Cantharidin is a topical agent, an inhibitor of phosphodiesterase, which produces an intraepidermal blister, followed by resolution of the lesion and healing without a scar. Potassium hydroxide is an alkaline compound that dissolves keratin.2 It has been used in concentrations and therapeutic schemes that vary from 5%to 20%, two times a day or every other day for 1 week or until inflammation develops. Other chemical methods reported are: podophyllotoxin, trichloroacetic acid, salicylic acid, lactic acid, glycolic acid, benzoyl peroxide, and tretinoin.
Phenol - Treatment with phenol has more risk of scarring. Phenol,however, is very commonly used world over as as an accepted form of treatment to treat molluscum lesions.
Immunomodulatory methods
Immunomodulatory methods stimulate the patient’s immune response against the infection. Imiquimod is an immunostimulatory agent that activates the innate and acquired immune response. The clinical effect of imiquimod stems from cytokine-induced activation of the immune system.
for more information about imiquad click here
References
-
Meza-Romero R, Navarrete-Dechent C, Downey C. Molluscum contagiosum: an update and review of new perspectives in etiology, diagnosis, and treatment. Clin Cosmet Investig Dermatol. 2019 May 30;12:373-381. doi: 10.2147/CCID.S187224. PMID: 31239742; PMCID: PMC6553952.
-
Weller R, O'Callaghan CJ, MacSween RM, White MI. Scarring in Molluscum contagiosum: comparison of physical expression and phenol ablation. BMJ. 1999 Dec 11;319(7224):1540. doi: 10.1136/bmj.319.7224.1540. PMID: 10591712; PMCID: PMC28297.
- Puri N. A study on the use of imiquimod for the treatment of genital molluscum contagiosum and genital warts in female patients. Indian J Sex Transm Dis AIDS. 2009 Jul;30(2):84-8. doi: 10.4103/0253-7184.62763. PMID: 21938126; PMCID: PMC3168064.