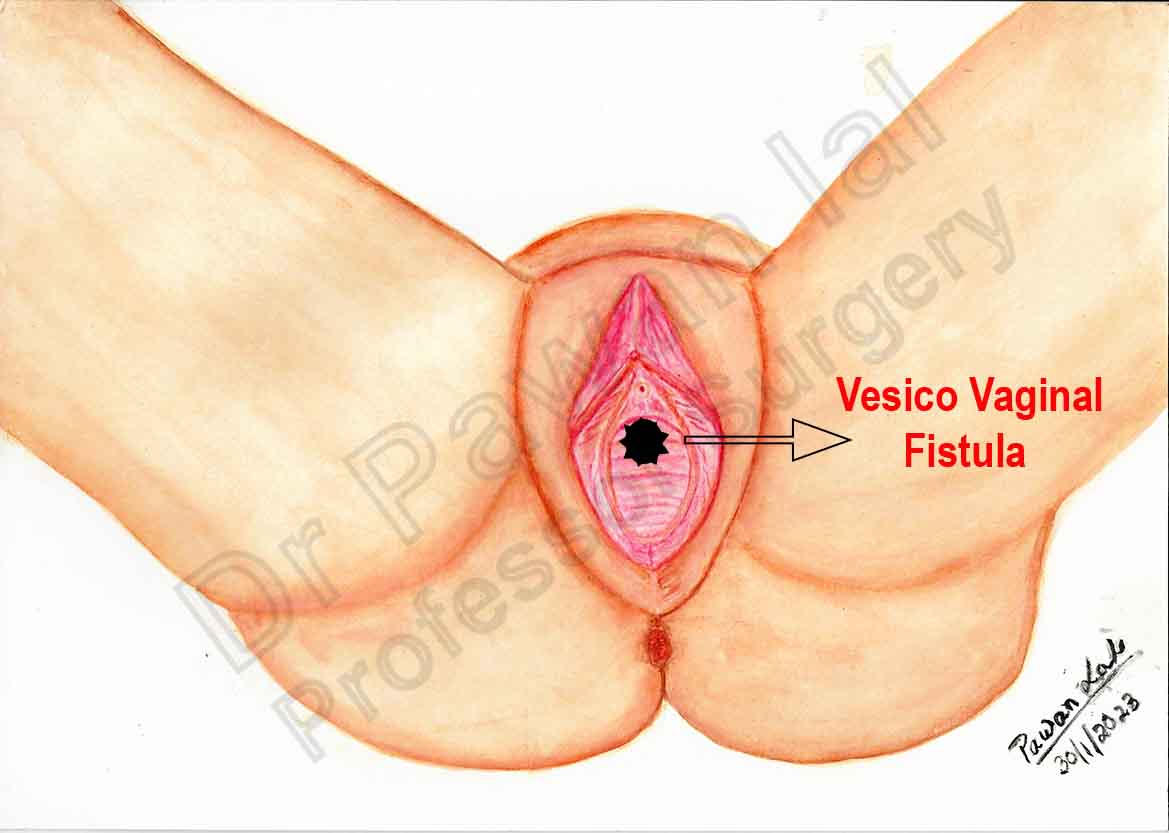
Anatomy of Vesico-Vaginal Fistula

Female external genitalia comprises of both urinary and reproductive structures, which collectively are called as vulva. The vulva (plural: vulvas or vulvae) is a term derived from Latin which means a wrapper or covering. The external genitalia are wrapped or covered by skin folds called labia majora and labia minora which are part of vulva. The vulva consists of the mons pubis, labia majora, labia minora, clitoris, urethra, vulva vestibule, vestibular bulbs, Bartholin's glands, Skene's glands, and vaginal opening.
Vulva
The vulva is the global term that describes all of the structures that make the female external genitalia. The components of the vulva are the mons pubis, labia majora, labia minora, clitoris, vestibular bulbs, vulva vestibule, Bartholin's glands, Skene's glands, urethra, and vaginal opening.
Vagina
The vagina is an elastic, muscular tube connected to the cervix proximally and extends to the external surface through the vulva vestibule. The term Vagina comes from the Latin for “sheath,”
The vaginal introitus is equivalent to the Level III section of the vagina, measured posteriorly from the clitoris to the anterior perineum then down the perineum to the anal verge. The anterior and posterior vestibules, with nonkeratinizing epithelium, extend laterally to the keratinized epithelium of the labia minora (Hart's line)2.
Level III of the vagina, that is, those areas distal to the hymen, anterior, lateral and posterior. It incorporates the
- anterior vestibule: anterior and lateral areas distal to the hymen. Laterally, it extends as far as Hart's line where the labia minora commence;
- Posterior vestibule: posterior and posterolateral areas distal to the hymen out to Hart's line;
- The perineum (predominantly anterior aspects), from distal margin of posterior vestibule down to anal verge.
The word “vestibule” comes from the Latin “vestibulum” meaning “a small cavity or a space at the entrance of a canal.
The distal opening of the vagina is usually partially covered by a membrane called the hymen. The vaginal opening is located posterior to the urethra opening. The function of the vagina is for sexual intercourse and childbirth. During sexual intercourse, the vagina acts as a reservoir for semen to collect before the sperm ascending into the cervix to travel towards the uterus and fallopian tubes. Also, the vagina also acts as an outflow tract for menses.
- Hits: 75
Etiopathogenesis and Classification of VVF
Classification

Simple fistulas are usually small in size (≤0.5cm) and are present as single non-radiated fistulas.
Complex fistulas include previously failed fistula repairs or large-sized (≥2.5 cm) fistulas, fistulas due to chronic diseases or radiotherapy and fistulas more than 2.5 cm in size.
Causes of Vesico-Vaginal Fistulas
- Traumatic
- Postsurgical - Abdominal or vaginal hysterectomy
- External trauma (e.g., penetrating, pelvic fracture, sexual assault)
- Radiation therapy
- Advanced pelvic malignancy
- Foreign body
- Obstructed labour
- Uterine rupture
- Caesarean section injury to bladder
- Congenital
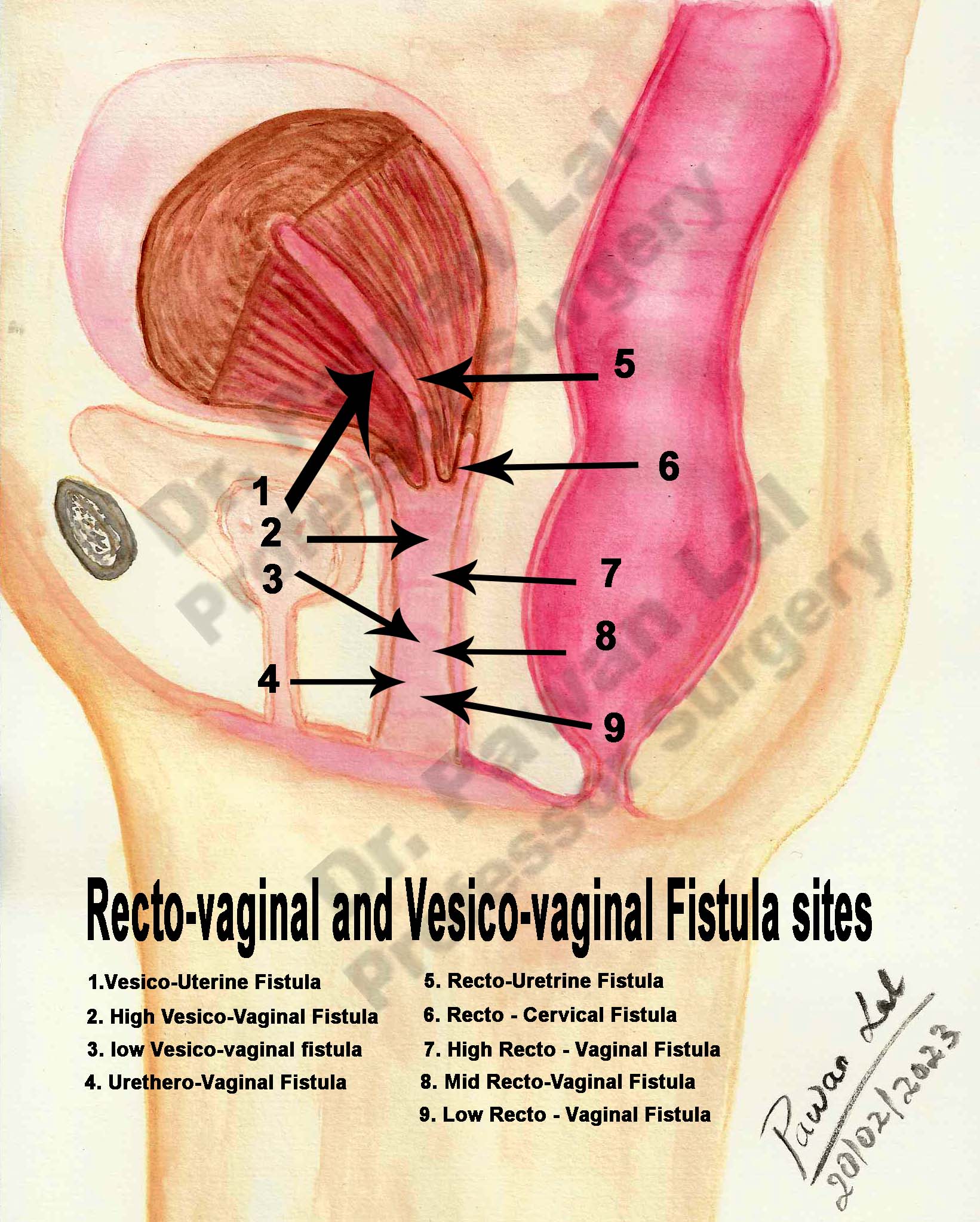
Classification
Marion Sims Classification (1852)
- Urethro-vaginal
- Bladder neck
- Body and floor of bladder
- Utero-vesical
Waaldijk Classification (1995).
Type 1 fistula – not involve closing mechanism
Type 2 – involve closing mechanism
-
-
without (sub)total urethra involvement
- with (sub)total urethra involvement
- without circumferential defect
- with circumferential defect
-
Type 3 – ureter and other exceptional fistula
GOH Classification 1
Type 1: Distal edge of fistula > 3.5 cm from external urinary meatus
Type 2: Distal edge of fistula 2.5–3.5 cm from external urinary meatus
Type 3: Distal edge of fistula 1.5 − < 2.5 cm from external urinary meatus
Type 4: Distal edge of fistula < 1.5 cm from external urinary meatus
-
- Size < 1.5 cm, in the largest diameter
- Size 1.5–3 cm, in the largest diameter
- Size > 3 cm, in the largest diameter
i. None or only mild fibrosis (around fistula and/or vagina) and/or vaginal length > 6 cm, normal capacity
ii. Moderate or severe fibrosis (around fistula and/or vagina) and/or reduced vaginal length and/or capacity
iii. Special consideration e.g. postradiation, ureteric involvement, circumferential fistula, previous repair.
Rosenshein (1980) (genito-anorectal classification)
i. Type 1: Total loss of perineal body with no other associated defects
ii. Type 2: Fistula associated with loss of perineal body
iii. Type 3: Fistula in lower third of vagina, intact or attenuated perineal body
iv. Type 4: Fistula in middle third of vagina
v. Type 5: Fistula in upper third of vagina
Presentation
The classical presentation sign is continuous (day and night) incontinence after a recent pelvic operation. If the fistula is small, then watery discharge from the vagina accompanied by normal voiding may be the only symptom. The patient may experience recurrent cystitis or pyelonephritis; unexplained fever; hematuria; flank, vaginal, or suprapubic pain; and abnormal urinary stream. Those with larger fistulas may not void transurethrally and may have total incontinence. Urinary leakage may make the patient a social recluse, disrupt sexual relations, and lead to depression, low self-esteem, and insomnia. The leakage of urine may cause irritation of the vagina and vulvar mucosa, and perineum and usually produces a foul ammonia odor.
References
1. Goh JT. A new classification for female genital tract fistula. Aust N Z J Obstet Gynaecol. 2004 Dec;44(6):502-4. doi: 10.1111/j.1479-828X.2004.00315.x. PMID: 15598284.
- Hits: 60
Investigations for VVF
Usually, fistulas occur between the 7th and 12th day after obstetric or gynecologic surgery. The diagnosis can be established by filling the bladder with a dilute solution of methylene blue. In a patient with urinary incontinence, the tampon test, where a tampon is inserted into the vagina after filling the bladder with the solution and the patient is ambulated, can lead to the confirmation of diagnosis. Cystoscopy is also of particular help and can clarify the exact anatomic origin. For small fistulas, it may be helpful to attempt to pass a small ureteric catheter through the suspected fistula tract to determine if it enters the vagina.
- Hits: 57
Management of VVF
Management
The operative techniques are described as Abdominal or vaginal approaches
The timings of repair of Vesico-Vaginal Fistula
- Obstretic fistula - 3 to 6 months delay before definitive repair
- Post radiation Fistula - 6 to 12 months delayed repair
- Post abdominal surgery - abdominal approach - 3 months preferable while vaginal approach 2 to 3 weeks after initial surgery.
Abdominal Approach (O'Connor's Technique)
Vaginal approach
- Martius interposition flap - In 1928 Martius described a labial flap of bulbocavernosus muscle for urethrovaginal fistula repair, which was later modified multiple times, and in modern usage generally refers to a labium majora fat pad flap without muscle. The Labia Majora incision is given on most prominent part and labial fat pad dissected (which is brigh yellow fibrofatty tissue). There is a natural tissue plane around the fibrofatty fatpad. Care has to be taken that the poserior lateral attachment through which blood supply from a branch of internal pudendal is present is not damaged. Posterior dissection is then performed and fibrofatty fat pad freed from the proximal attachment. A length of 8 to 15 cm can be easily mobilized in this fibro-fatty fat pad, the length should be adequate and there should be no tension in the repair. Care should be taken to stay lateral to the bulbocavernosus and ischiocavernosus muscles. Too medial a dissection includes these structures and results in significant bleeding. Too superficial a dissection risks scar deformity.

Conservative management
Surgical Therapy
Surgical objectives or principles
Tips
- for Martius flap - put foley's catheter plastic sheath over the Martius Flap and the flap slides very easily into the tunnel
- Trans-labial ultrasound for decent of bladder and angle of bladder for stress incontinence
- TVT vs TOT
- Overactive bladder inject botulinium toxin in trigone of bladder (Trans-vaginal) or trans-vesical
- Overactive bladder - sacral biomodulation / Sacral neuromodulation
- Bladder pressure - 40 mm Hg of water is cut off after which damage to kidneys start occurring
Post-operative care
References:
- Wilson A, Pillay S, Greenwell T. How and why to take a Martius labial interposition flap in female urology. Transl Androl Urol. 2017 Jul;6(Suppl 2):S81-S87. doi: 10.21037/tau.2017.04.38. PMID: 28791226; PMCID: PMC5522801.
- Hits: 58
Pyschological impact of VVF on patient
Tears of Childbirth
Motherhood is expected to be a time of joy but women often die or develop complications, such as obstetric fistula during the process of child-bearing. Obstetric fistula is regarded as the most devastating of all childbirth related morbidities.
Obstetric fistula patients present for repair surgery with more severe psychological distress than gynecology outpatients. In order to address these mental health concerns, clinicians should engage obstetric fistula patients with targeted mental health interventions.
Women reported many psychological consequences of VVF including depression, feelings of shame, and loneliness. Others reported feeling devalued as a woman and wanting to end their lives
- Hits: 108
